Introduction
Have you ever experienced dry, irritated eyes that just won’t seem to go away? You’re not alone. Dry eye syndrome is a common condition that affects millions of people worldwide, and your eye doctor and optometrist wants you to be informed. Understanding the symptoms and causes of dry eye can help you take better care of your ocular health and seek timely treatment when needed.
Dry eye syndrome is a common condition that affects millions of people worldwide, and your eye doctor and optometrist wants you to be informed. Understanding the symptoms and causes of dry eye can help you take better care of your ocular health and seek timely treatment when needed.
In this article, we’ll explore the anatomy of tears and delve into the common symptoms of dry eye. You’ll learn about the factors that contribute to this condition and discover modern approaches to treatment. Whether you’re dealing with occasional discomfort or chronic dryness, your optometrist or eye care provider has valuable insights to share about diagnosis, eye drops, and other strategies to keep your eyes feeling comfortable and healthy.
The Anatomy of Tears
To understand dry eye syndrome, it’s crucial to grasp the intricate structure and function of tears. 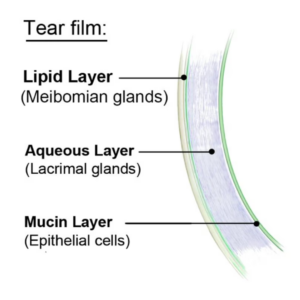 Your tears are more complex than you might think, playing a vital role in maintaining your eye health and vision.
Your tears are more complex than you might think, playing a vital role in maintaining your eye health and vision.
Tear Film Composition
Your tear film is a thin, protective coating that covers the surface of your eyes. It’s made up of three distinct layers, each with its own unique purpose 1:
- Oil (Lipid) Layer: This outer layer helps seal the tear film, reducing evaporation of your natural tears.
- Water (Aqueous) Layer: The middle and thickest layer, it lubricates your eye, washes away particles, and helps prevent infection.
- Mucin Layer: The innermost layer allows the watery layer to spread evenly over your eye’s surface, ensuring proper lubrication and nourishment of the cornea.
The tear film is remarkably thin, measuring only about 3 μm in thickness, with a volume of approximately 3 to 10 μL 2. It’s continuously produced at a rate of 1 to 2 μL per minute to maintain its protective properties.
Function of Tears
Your tears serve several essential purposes 1:
- Protection and lubrication of the eyes
- Reduction of infection risk
- Removal of foreign particles
- Maintenance of a smooth and clear eye surface
The tear film contains various components that contribute to these functions. For instance, the aqueous layer houses proteins, metabolites, inorganic salts, glucose, oxygen, and electrolytes such as magnesium, bicarbonate, calcium, and urea 2. These elements are crucial for maintaining your ocular surface health and flushing away debris and toxins.
For instance, the aqueous layer houses proteins, metabolites, inorganic salts, glucose, oxygen, and electrolytes such as magnesium, bicarbonate, calcium, and urea 2. These elements are crucial for maintaining your ocular surface health and flushing away debris and toxins.
Additionally, your tears have antimicrobial properties. Key factors like lysozyme, lactoferrin, transferrin, and various immunoglobulins found in the aqueous layer help defend your eyes against potential infections 2.
Tear Production Process
Your body produces three types of tears 3:
- Basal tears: These are always present in your eyes, providing constant protection and lubrication.
- Reflex tears: Produced in response to irritants like smoke or onion fumes.
- Emotional tears: Generated when you experience intense emotions, whether happy or sad.
The process of tear production and distribution is fascinating. When you blink, tears spread across the surface of your eye. They then drain into small holes in the corners of your upper and lower lids before traveling through channels and down your tear ducts to your nose 3.
Interestingly, tear production is regulated by your nervous system. Sensory neurons in your cornea and eyelids respond to temperature changes and irritants through various receptors. This triggers parasympathetic activation, leading to increased aqueous and mucin production. Sympathetic inputs also play a role, stimulating secretion from conjunctival epithelial cells 2.
As you age, your tear production may slow down, particularly the production of basal tears. This is why dry eye syndrome is more common in older adults, especially women after menopause due to hormonal changes 3. However, it’s important to note that you don’t actually run out of tears – your body continues to produce them, just at a reduced rate.
However, it’s important to note that you don’t actually run out of tears – your body continues to produce them, just at a reduced rate.
Understanding the complex anatomy and function of your tears can help you appreciate the importance of maintaining good eye health and seeking proper care when you experience symptoms of dry eye.
Common Dry Eye Symptoms
Dry eye syndrome, also known as dry eye disease or keratoconjunctivitis sicca, is a multifaceted condition that can cause a range of uncomfortable symptoms 4. Understanding these symptoms can help you recognize when it’s time to consult your optometrist. Let’s explore the most common signs of dry eye:
Ocular Discomfort
One of the hallmark symptoms of dry eye is a persistent feeling of discomfort in your eyes.  This can manifest in several ways:
This can manifest in several ways:
- Stinging or burning sensation
- Feeling of pressure in your eyes
- Sandy or gritty sensation, as if something is stuck in your eye 4
- Sharp or dull pain, which can be localized to a specific part of your eye or even around the orbit 4
- Redness, which may worsen with the use of over-the-counter eye drops containing vasoconstrictors 4
- Heavy eyelids or difficulty opening your eyes
- Excessive blinking or eyelid twitching 4
You might also experience tired eyes, finding relief when you close them. In severe cases, you may even have difficulty crying 4.
Vision Changes
Dry eye can also affect your vision in various ways:
- Blurry vision, particularly intermittent blurriness
- Glare or halos around lights, especially at night 4 5
- Fluctuating vision and difficulties in reading 4
- Increased sensitivity to light 6
These vision changes occur because an inadequate or poor-quality tear film can interfere with the way light enters your eye, affecting your ability to see clearly 5.
Excessive Tearing
Surprisingly, one of the symptoms of dry eye is excessive tearing or watery eyes. This might seem counterintuitive, but there’s a logical explanation:
When your eyes are dry, it can lead to irritation. In response, your lacrimal glands may produce an abundance of tears to try to alleviate the discomfort. However, these excess tears are often of poor quality and don’t effectively lubricate your eyes 6.
In response, your lacrimal glands may produce an abundance of tears to try to alleviate the discomfort. However, these excess tears are often of poor quality and don’t effectively lubricate your eyes 6.
This happens because the meibomian glands, responsible for producing the oily layer of your tear film, aren’t functioning properly. Without enough oil, the watery part of your tears evaporates too quickly. Your body tries to compensate by producing more watery tears, but these can’t properly coat your eye surface 6.
It’s important to note that dry eye can also cause other symptoms:
- Mucus discharge from your eyes 6
- Difficulty wearing contact lenses comfortably 4
- A feeling that your eyelids are stuck together upon waking
Interestingly, a 2016 study found a connection between poor sleep quality and dry eye disease in adults aged 26-64 5. This highlights the complex nature of dry eye and its potential impact on various aspects of your daily life.
If you’re experiencing any combination of these symptoms, it’s crucial to consult your optometrist. They can provide a proper diagnosis and recommend appropriate treatment options to help alleviate your discomfort and improve your eye health.
They can provide a proper diagnosis and recommend appropriate treatment options to help alleviate your discomfort and improve your eye health.
Factors Contributing to Dry Eye
Age-Related Changes
As you age, your risk of developing dry eye increases significantly. Studies have shown that the prevalence of dry eye rises every five years after the age of 50, with women being more affected than men 7. This increased risk is due to several age-related changes in your eyes and surrounding structures.
Your lacrimal gland, responsible for tear production, undergoes various histopathologic changes as you age. These include acinar atrophy, fibrosis, and lymphocytic infiltration 7. These alterations can lead to decreased tear production, contributing to dry eye symptoms.
Additionally, age-related eyelid changes such as lid laxity and meibomian gland atrophy can affect tear distribution and quality 7.  These changes, combined with decreased corneal sensitivity that occurs with aging, can predispose you to dry eye 8.
These changes, combined with decreased corneal sensitivity that occurs with aging, can predispose you to dry eye 8.
Environmental Influences
Your environment plays a crucial role in the development and exacerbation of dry eye symptoms. Warm or dry air can cause moisture to evaporate from the surface of your eyes more quickly, making you more prone to dry eye 9. This is why people living in hot, dry climates often experience year-round dry eye symptoms.
Warm or dry air can cause moisture to evaporate from the surface of your eyes more quickly, making you more prone to dry eye 9. This is why people living in hot, dry climates often experience year-round dry eye symptoms.
Air pollution, dust, and smoke can also contribute to dry eye. These tiny particles can lodge themselves in your tear film, reducing its ability to keep your eyes lubricated 9. Moreover, pollutants can trigger inflammation on the surface of your eyes, affecting tear production and quality.
Indoor environments can be equally problematic. Poor air quality from indoor pollution, dust, or cigarette smoke is linked to dry eye 9. Even activities like prolonged computer use or reading can contribute to dry eye by reducing your blink rate 10.
Medical Conditions
Various medical conditions can increase your risk of developing dry eye. Autoimmune diseases such as Sjögren’s syndrome and rheumatoid arthritis are known to affect tear production 8. Other conditions like diabetes mellitus can impact your lacrimal gland function and corneal nerves, leading to dry eye symptoms 7.
Neurodegenerative diseases, particularly Parkinson’s disease, can predispose you to evaporative dry eye 8. This is due to reduced blinking, which affects tear distribution across the eye surface.
It’s important to note that many medications commonly prescribed for age-related conditions can cause or exacerbate dry eye. These include antidepressants, diuretics, dopaminergic drugs for Parkinson’s disease, and antimetabolites used in treating rheumatoid arthritis 8. Even over-the-counter medications and supplements can contribute to dry eye symptoms, especially in older adults 8.
Topical medications, such as those used to treat glaucoma, can also increase your risk of developing dry eye 8. As glaucoma is more prevalent in older adults, this risk factor becomes increasingly relevant with age.
Understanding these contributing factors can help you and your optometrist develop a comprehensive approach to managing dry eye, addressing both internal and external influences on your eye health.
Modern Approaches to Dry Eye Treatment
 Artificial Tear Supplements
Artificial Tear Supplements
Artificial tears are a cornerstone in managing dry eye disease. These supplements aim to enhance your tear film and provide relief from symptoms 11. While they may not address the underlying causes, artificial tears have shown to improve both symptoms and certain signs of dry eye 11.
You’ll find a wide variety of artificial tear formulations available, each with unique properties such as viscosity, osmolarity, and additional ingredients like osmoprotectants and lipids 11. Some formulations have higher viscosity, like ointments and gels, which are designed to stay on your eye surface longer but may temporarily blur your vision 11.
When choosing artificial tears, you might want to consider preservative-free options to avoid potential ocular surface changes associated with preservatives 11. Studies have shown that artificial tears can significantly improve dry eye symptoms. For instance, a study of 394 patients showed an approximately 16-point improvement in the Ocular Surface Disease Index (OSDI) score after 90 days of using artificial tears 11.
However, it’s important to note that not all patients benefit from artificial tears. In one study, about 26% of patients didn’t respond to treatment, and some even experienced worsening symptoms 11. If you don’t see improvement after a month of consistent use, it’s advisable to consult your optometrist about alternative treatments 12.
Prescription Eye Drops
When over-the-counter artificial tears aren’t enough, your optometrist may recommend prescription eye drops. These medications are specifically designed to target the underlying causes of dry eye disease.
- Restasis and Cequa: These drops contain cyclosporine, which helps reduce inflammation and increase natural tear production 13. They’re typically prescribed to be taken twice a day, but it may take 3 to 6 months before you notice significant improvement 13.
- Xiidra: This medication uses lifitegrast to decrease inflammation 13. It’s also taken twice daily but may show results more quickly, in as little as one month 13.
- Eysuvis: This is the first FDA-approved ocular corticosteroid for treating dry eye flares 14. It’s used for short-term treatment, typically for two weeks at a time 14.
In-Office Procedures
For more severe cases of dry eye, your optometrist may recommend in-office treatments. These procedures can provide longer-lasting relief and target specific causes of dry eye.
- Intense Pulsed Light (IPL) Therapy: Originally used for skin rejuvenation,
 IPL is now applied to treat dry eye syndrome 15. It works by closing blood vessels that secrete inflammatory proteins, helping to improve meibomian gland function 15.
IPL is now applied to treat dry eye syndrome 15. It works by closing blood vessels that secrete inflammatory proteins, helping to improve meibomian gland function 15. - LipiFlow: This FDA-cleared thermal pulsation treatment addresses evaporative dry eye disease 15. The 12-minute procedure applies heat and gentle pressure to your eyelids, unblocking meibomian glands and encouraging natural oil production 15.
- Punctal Plugs: These tiny devices are inserted into your tear ducts to prevent tears from draining too quickly, helping to keep your eyes moisturized 16.
- Amniotic Tissue Treatment: This innovative approach has shown promising results, providing comfort for severely dry eyes for months after treatment 16.
Remember, the most effective treatment plan for your dry eyes will depend on your specific condition and symptoms. Your optometrist can help determine the best approach for you, which may involve a combination of these modern treatments.
Conclusion
Dry eye syndrome is a complex condition that has a significant impact on millions of people worldwide.  This article has shed light on the intricate anatomy of tears, the common symptoms of dry eye, and the various factors that contribute to this condition. From age-related changes to environmental influences and medical conditions, understanding these aspects is crucial to manage and treat dry eye effectively.
This article has shed light on the intricate anatomy of tears, the common symptoms of dry eye, and the various factors that contribute to this condition. From age-related changes to environmental influences and medical conditions, understanding these aspects is crucial to manage and treat dry eye effectively.
Modern approaches to treat dry eye offer hope to those suffering from this condition. From artificial tear supplements and prescription eye drops to cutting-edge in-office procedures, there are now more options than ever to alleviate symptoms and improve eye health. Remember, the key to finding relief lies in working closely with your optometrist to develop a tailored treatment plan that addresses your specific needs and symptoms.
FAQ
- Can an optometrist provide treatment for dry eye syndrome?
- Yes, optometrists can treat dry eye syndrome. The goal of treatment is to replenish or maintain the normal tear levels in the eyes, reducing dryness and discomfort while preserving eye health. Even though dry eye can be a long-term issue, effective treatments are available through optometrists.
- What type of eye drops do eye care providers suggest for dry eyes?
- For cases of evaporative dry eye, eye care providers often recommend eye drops that contain lipid- or oil-based components. These ingredients help thicken the tear film and prevent it from evaporating too quickly. When choosing eye drops, look for products that include oils in their ingredients list or specifically mention treatment for evaporative dry eye.
- What general care advice is recommended for managing dry eyes?
- Managing dry eyes can often be effectively handled with regular eyelid cleaning and the use of over-the-counter eye drops or other lubricating products. If you have chronic dry eye, it’s advisable to use eye drops regularly, even when your eyes do not feel dry, to maintain proper lubrication.
- Should I consult an optometrist or an ophthalmologist for dry eye issues?
- For common problems such as dry eyes, redness, or minor vision issues, optometrists are well-equipped to provide treatment and care. They are also recommended for regular annual eye examinations. Optometrists have the necessary training and experience to manage these conditions effectively. If treatment requires surgical or serious intervention your eye care provider will refer you to an ophthalmologist.
References
[1] – https://www.refreshbrand.com/dryeye/tear-film
[2] – https://www.ncbi.nlm.nih.gov/books/NBK572136/
[3] – https://www.healthline.com/health/what-are-tears-made-of
[4] – https://www.ncbi.nlm.nih.gov/books/NBK470411/
[5] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7672346/
[6] – https://my.clevelandclinic.org/health/diseases/24479-dry-eye
[7] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5347479/
[8] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4150485/
[9] – https://www.webmd.com/eye-health/dry-eye-irritants
[10] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10482047/
[11] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9704006/
[12] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9840372/
[13] – https://premiereye2020.com/3-common-prescriptions-eye-drops-for-dry-eye/
[14] – https://www.aao.org/eye-health/tips-prevention/new-dry-eye-treatments-ocular-surface-disease
[15] – https://www.matossianeye.com/dry-eye-in-office-treatments/
[16] – https://www.optometrists.org/general-practice-optometry/guide-to-eye-conditions/dry-eye/10-in-office-treatments-for-dry-eyes/